Preparing for medical decision making is not only about peace of mind, it is about giving doctors and loved ones clear instructions they can honor without guesswork. Two documents do most of the heavy lifting in Texas: a directive to physicians, commonly called a living will, and a medical power of attorney. Together they set the guardrails for care if you cannot speak for yourself and name the person who can speak with your doctor on your behalf.
In this guide, we’ll explain what each document does under Texas law, how they work together in real situations, and how you can complete, store, and keep them current. You will also see practical choices to think through now so your paperwork reflects your values when it matters.
- What a Living Will Means Under Texas Law
- How Advance Directives Work With Medical Power of Attorney and DNR
- When These Documents Apply and When They Do Not Orders
- How to Complete the Forms Correctly in Texas
- Choosing and Preparing Your Health Care Agent
- How to Update or Revoke Without Confusion
- Common Mistakes and How to Avoid Them
- Using the Phrase Advance Directive and Living Will Accurately
- Real World Scenarios That Test Your Paperwork
What a Living Will Means Under Texas Law
Texas uses the term Directive to Physicians and Family or Surrogates. It is a written statement that tells your physician whether you want life sustaining treatment provided, withheld, or withdrawn if you are in a terminal condition or an irreversible condition and cannot communicate informed choices. The statutory form gives you options to accept or refuse treatment that only prolongs the process of dying, and it lets you address artificial nutrition and hydration specifically. Comfort care is always allowed.
Key points to understand:
- The scope is limited to terminal or irreversible conditions as certified by a physician.
- You can state preferences about ventilation, CPR, dialysis, antibiotics, blood products, and tube feeding, and you can add instructions in your own words.
- Your wishes guide care even if family members disagree, since the document speaks directly to the physician.
- A living will does not control routine care or ordinary treatment when you are expected to recover.
Texas public policy has special rules related to pregnancy. If you are pregnant, certain life sustaining treatments may continue regardless of a directive. This is set by statute and providers must follow it.
How Advance Directives Work With Medical Power of Attorney and DNR Orders
An advance directive is an umbrella term that covers several tools. The two most common are the living will and the medical power of attorney. The medical power of attorney names an agent to make health care decisions any time you lack capacity, not only at end of life. Your agent must follow your known wishes, and a clear living will helps the agent and your physician apply those wishes in complex cases.
A do not resuscitate order is different. A DNR tells clinicians not to attempt CPR if your heart or breathing stop. In the hospital it is a physician order placed in your chart. Outside the hospital, an out of hospital DNR must meet state rules so EMS can honor it, which usually includes a signed form or authorized bracelet or necklace. Many people complete both a living will and a medical power of attorney, then discuss with their physician whether a DNR is appropriate given their health status.
Think of it this way. Your living will states your goals for treatment in defined conditions, your medical power of attorney appoints the person who applies those goals across situations, and DNR status is a clinical order that translates your wishes into bedside action during a cardiopulmonary arrest.
When These Documents Apply and When They Do Not
Capacity is the first gate. If you can understand information and communicate a choice, you decide for yourself. If you lack capacity, your medical power of attorney agent steps in. If you are also in a terminal or irreversible condition, your living will becomes a binding expression of your preferences. If there is no living will, your physician turns to the agent, or if no agent exists, to the surrogate hierarchy in state law.
These documents do not control:
- Routine care for short term, self limited problems when you have capacity
- Mental health admission decisions or certain invasive psychiatric treatments that agents are not allowed to authorize
- Requests that would require a clinician to provide care that is outside medical standards
Texas law also lays out a process for ethical review when there is a conflict between a requested treatment and medical judgment. The timelines and notice requirements are prescribed, and your agent will receive information about transfer options if that process is used.
How to Complete the Forms Correctly in Texas
The state provides model forms that are widely used and accepted. Use current versions so your doctor and hospital staff can recognize them immediately.
Signing rules to follow:
- Living will. Sign and date it in the presence of two qualified adult witnesses, or sign before a notary. At least one witness must not be related to you, must not be entitled to any part of your estate, must not be your attending physician or an employee of the facility providing care, and must not have any claim against your estate.
- Medical power of attorney. You can sign before a notary or two qualified witnesses with similar restrictions. Your named agent cannot be a witness.
If you cannot sign, you can direct another person to sign for you in your presence. Keep signatures legible and dates clear. Do not alter statutory language with cross outs. If you add instructions, use the space provided or a clearly labeled addendum and initial each page.

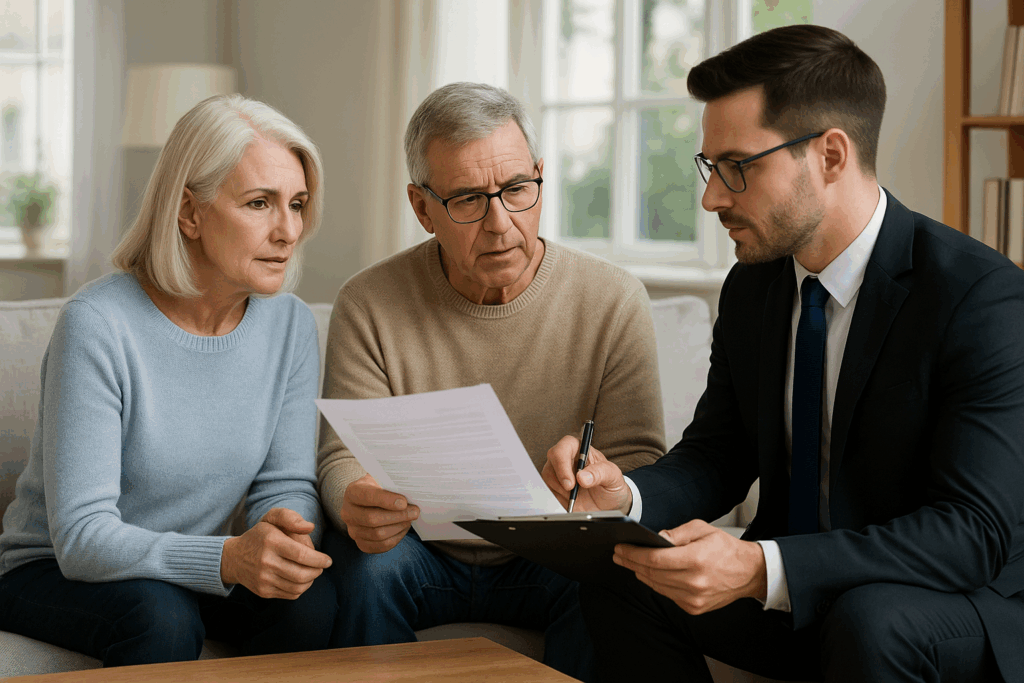
Choosing and Preparing Your Health Care Agent
Your agent should be calm under pressure, willing to follow your stated wishes even if others disagree, and able to speak plainly with clinicians. You can name one primary agent and at least one alternate. You cannot name your health care provider or an employee of your provider unless that person is a relative.
Limits of agent authority include the following. An agent cannot consent to voluntary inpatient mental health services for you, cannot agree to convulsive treatment or psychosurgery, and cannot consent to abortion. Your agent is also bound by your living will and any instructions you wrote. If a choice is not covered by your writing, your agent should decide based on your values and goals that you have discussed with them in advance.
Prepare your agent by holding a real conversation. Cover what quality of life means to you, how you feel about time in the ICU, how long you would want to remain on a ventilator if recovery is unlikely, and how you view artificial nutrition and hydration in the setting of poor prognosis. The more specific you are, the easier your agent’s task will be.
Making Treatment Choices Specific and Practical
Vague statements like do everything or no machines often create confusion. Translate values into choices your physician can follow. Consider the following prompts as you draft your living will and talk with your agent:
- If my brain injury or dementia leaves me permanently unable to recognize family or interact meaningfully, I would or would not want artificial nutrition and hydration.
- If I have a terminal cancer with short life expectancy despite treatment, I would accept, limit, or refuse another trial of ventilation or ICU care.
- If I am likely to die from my illness within a short time and CPR would not restore meaningful recovery, I would or would not want CPR attempted.
- I want comfort care to be prioritized, including pain control and relief of shortness of breath, even if that may shorten life.
You can also add directions about organ and tissue donation, spiritual care, and who you want included in conference calls or bedside discussions.

A beautifully drafted form does no good if no one can find it. Keep the original in a place that is easy to reach, not in a safe deposit box. Give copies to your agent, alternates, primary care physician, the specialist who manages your serious condition, and your preferred hospital. Ask each provider to scan the forms into your electronic record. Carry a wallet card that lists your agent’s contact details and states that you have a medical power of attorney and a living will. If you use a patient portal, upload the PDFs to the documents section.
If you spend time across state lines, carry the Texas forms and consider completing a simple state neutral set that references your Texas documents. Hospitals in other states usually honor clear instructions, but having familiar paperwork reduces delays.
How to Update or Revoke Without Confusion
You can revoke a living will at any time by destroying the document, by signing a written revocation, or by telling your physician that you revoke it. You can revoke a medical power of attorney by notifying your agent or physician, by executing a new medical power of attorney, or by any act that clearly shows intent to revoke. If you divorce, any designation of your former spouse as agent is no longer effective unless you reappoint them later.
When you update, replace every copy. Email a fresh PDF to your agent and alternates on the same day you sign. Ask your physicians to archive the old version and upload the new one. Put a new wallet card in your bag or phone case. Do not keep multiple versions in circulation.
Common Mistakes and How to Avoid Them
- Leaving artificial nutrition and hydration blank. Address it directly so no one has to guess.
- Picking an agent only by seniority in the family. Choose the person most likely to follow your wishes and communicate well.
- Signing without qualified witnesses or a notary. Follow the exact rules so no one questions validity during a crisis.
- Filing the forms and never speaking about them. A short, candid talk with your agent and family reduces conflict later.
- Forgetting to align orders with preferences. If your goals support a DNR in the current clinical picture, ask your physician to write the order and make sure it appears in your chart.
When to Consult an Attorney and What to Ask
The state forms are designed for personal use. Many people complete them without counsel. An attorney can still help when you have blended families, a history of disputes, a rare diagnosis with complex interventions, or questions about how these documents interact with your broader estate plan.
If you choose to hire counsel, focus your consult by asking:
- Does my wording about life sustaining treatment match Texas statutory terms so clinicians can apply it without delay
- How should my medical power of attorney reference my living will so the agent’s authority and my instructions are fully aligned
- What HIPAA language should I add to ensure my agent can access records quickly
- How should I coordinate a DNR or a portable medical order with my physician so EMS and hospital staff see the same plan
Using the Phrase Advance Directive and Living Will Accurately
People often use the terms as if they were identical. The living will is one type of advance directive. The set also includes the medical power of attorney and the out of hospital DNR under Texas law. When someone asks whether you have an advance directive and living will, they usually mean the complete package along with your agent designation. For clarity, keep your forms together in one envelope or one PDF and label the files with the date you signed. This section intentionally uses the main keyword advance directive and living will to match common search phrasing while keeping terminology precise.
Real World Scenarios That Test Your Paperwork
Scenario One
You have a stroke that leaves you unable to speak for several days. You are not in a terminal or irreversible condition. Your medical power of attorney agent can authorize tests and treatment until you regain capacity. Your living will stays in the background.
Scenario Two
You are admitted with end stage heart failure. Two physicians agree your condition is terminal. Your living will says you do not want life sustaining treatment that only prolongs dying, and you decline artificial nutrition and hydration. Comfort care is provided, and your agent confirms that your wishes remain the same.
Scenario Three
You live with advanced dementia and cannot make medical decisions. You develop pneumonia and respiratory failure. Your living will addresses irreversible conditions and bars intubation if recovery to meaningful interaction is not expected. Your agent and physician focus on oxygen, comfort, and relief of distress rather than ventilation and ICU transfer.
In each situation, clear writing and a prepared agent make choices consistent and respectful.
Conclusion
Good planning lets your values guide care when your voice is muted. A living will documents end of life preferences in the exact terms Texas physicians use, and a medical power of attorney places a trusted person beside your doctors when real time choices arise. Thoughtful conversations, precise wording, proper signatures, and smart distribution make your plan usable across busy clinics, emergency rooms, and hospital wards. If your family structure or health picture is complex, consider a brief legal consult and a focused appointment with your physician to align orders with your paperwork. The phrase advance directive and living will often serves as shorthand for the whole toolkit, and with the right steps you can make that toolkit clear, current, and ready.
Other Related Posts
- Finding the Right Texas Special Needs Trust Lawyer for Your Family’s Future
- Is a Living Will Legally Binding and How It Works in Real Situations
- Key Benefits of Minor Guardianship in Texas: Legal Protection and Parental Support
- Creating a Living Will: A Clear Legal Framework for Your Future Care
- How to File for Temporary Guardianship the Right Way: What You Need to Know
- Understanding the Cost of Special Needs Trust for Long-Term Planning
- How to Set Up a Living Will: Step-by-Step Legal Planning Guide
- Texas Guardianship Attorney Services: Essential Legal Support for Families
- Special Needs Trust Medicaid Guide: Protecting Benefits Without Sacrificing Support
- dvance Directives vs Living Will: A Practical Comparison for Medical Planning
- Texas Court Guardianship Evaluation Process: How It Works and What to Expect
- What Is a Living Revocable Trust and Why It Can Strengthen Your Estate Plan
Frequently Asked Questions
A living will states your preferences for life sustaining treatment if you are in a terminal or irreversible condition and cannot decide for yourself. A medical power of attorney names the person who makes health care decisions for you any time you lack capacity, guided by your stated wishes.
Your physician must follow your valid directive and your known wishes. Family input is considered, but your written instructions control unless a specific legal rule applies.
For a living will, use two qualified adult witnesses or a notary. For a medical power of attorney, use a notary or two qualified witnesses. Follow the disqualifier list so the signatures are valid.
Hospitals usually accept clear copies while they place an original in the chart when practical. Keep clean PDFs ready to send, and ask your physician’s office to upload them to your record.
Clinicians treat to preserve life until they can assess capacity and reach an appropriate decision maker. If a condition meets the legal criteria and your wishes are known, the team aligns care with those wishes as soon as possible.